Michelle Kickham examines the science behind coeliac disease and looks at what the future may hold for those suffering with the condition…
Ah, Coeliac Disease. A pizza lover’s worst nightmare. If you actually have it, you know what it really is – a right pain in the behind. Eating in a restaurant becomes complicated, and you pray that the waitron knows what you’re talking about when mentioned (‘Okay so you can’t have gluten – can you have pasta? No? Okay, well we have this wonderful garden salad!’) and you inevitably succumb to the garden salad for dinner. It’s a nuisance, but unfortunately, it must be managed and treated by strict adherence to a gluten-free diet (GFD). Although cases of CD appear to be rising – many of these cases are self-diagnosed and inaccurate (thanks to the latest gluten-free ‘fad’) when in actuality, CD affects only about 1% of the general population.
Background
In order to understand CD, let’s get some background information covered first – I’ll keep it short and sweet. Our immune system is an extremely complex, yet sophisticated network of cells, proteins and other small molecules that work together to maintain health. I like to think of the immune system as the body’s own little army; always prepared and able to detect, hunt down and defeat the enemy – and most importantly, keep its allies safe. Here, the enemy could be a virus, bacterium or anything it sees as ‘foreign’ or ‘dangerous’. The body’s allies are of course your own cells, DNA and proteins – things we need to maintain life. Sounds pretty simple, right? Not so much. You’ll see why shorty…
When we get attacked by a dangerous assailant (a virus, for example) our body declares war, instructing the immune system to attack the invader. These attacks can be brought on by anti-bodies which mark the invader as dangerous, so that these specialised cells in our body eat up the dangerous invader (yep – some of our cells eat bacteria!). Some immune responses rely on T-cells (aka Killer T-Cells – awesome name, right?), which kill the invader through the release of toxic chemicals. This is how the immune system is supposed to work – but sometimes, things go wrong. The body gets confused – and sometimes, this causes problems.
So, what is it exactly?
Coeliac disease is an autoimmune disease – not an intolerance, allergy, or dietary choice (despite the recent gluten-free fad). It is a serious condition and if not treated correctly can lead to chronic malnutrition, osteoporosis cancer of the small intestine. An auto-immune disease is when the body attacks its own cells either through antibodies or T-cells, leading to atrophy of tissue (organ damage), inflammation and in some cases, death. The pathophysiology (ie. the way in which the disease state manifests) of CD is still being researched and many aspects remain unclear, but the leading hypotheses (discussed below) support both a required genetic predisposition (meaning those with CD must have the specific genetic marker) and other triggers which may ‘turn on’ CD in those who previously showed no symptoms. Before we go into the hypotheses as to why we have it – let’s take a look at what happens to our body when we ingest gluten, and why it causes us so much damage.
What actually happens to us when we ingest gluten?
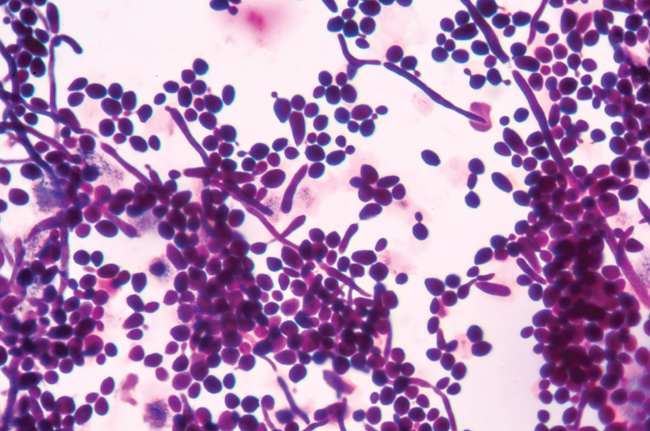
Coeliac disease is activated by peptides (small proteins) collectively termed as ‘gluten’ contained in wheat, barley, rye and spelt. The disease activating peptides are gliadin, glutenin, hordeins, and secalins. When someone with CD ingests gluten, it is modified by an enzyme called Tissue Transglutaminase (tTg) in such a way that makes it appears ‘dangerous’ to the immune system. These modified peptides are then taken up by specialised cells called Antigen Presenting Cells (APCs), which have ‘stages’ called MHC molecules (these are important) on their surface, where they display the antigen (in this case, “gluten”) to other immune cells, instructing them to attack the invader. When APCs present gluten to those killer T-cells, they begin to release toxic chemicals to destroy it – only, they also destroy the lining of our small intestine in the process! In addition, the body produces antibodies to mark gluten dangerous, resulting in an assault on both our own cells and anything gluten has come into contact with. Of course, what would an immune response be without chronic inflammation? Yep – we get all of that too. This inflammation arises due to the infiltration of immune cells to destroy the invader, gluten, and also to activate more cells to take part in the attack. Basically, all hell breaks loose in our intestine. The combinatory effect of this is villous atrophy (flattening of the villi; small protrusions in the gut which absorb nutrients from food) and the breakdown of the lining of the small intestine.

Symptoms and side-effects
The symptoms of CD are extremely diverse and range from mild gastrointestinal discomfort to complete malnutrition – depending on disease severity and frequency of exposure to gluten. However, most patients with CD present with the typical gastrointestinal problems such as diarrhoea and abdominal distension, skin issues such as dermatitis, fat soluble vitamin deficiencies (such as vitamin D and K) and cognitive issues such as difficulties in concentrating and memory retention. If left untreated, CD can lead to cancer of the colon and small intestine – which can be fatal. Chronic malnutrition as a result of CD often leads to osteoporosis (weakening of the bones), infertility and anaemia.
Why do I have it?
The precise cause of CD is still unclear, as it appears to be a lot more complex than some other autoimmune disorders. Although much is still to be learned, here is a run-down of the most recent hypotheses.
Genetics
As with most autoimmune disorders, CD is found only in those with a genetic predisposition – meaning you must have the specific genes in order to present with true CD. There are at least 250 genes involved in CD, but the main players are HLA-DQ2/8 – which are found in all coeliacs. These HLA genes are in charge of structures on the surface of your cells (called MHC molecules) and determine what they will bind or ‘stick to’, and how well they can bind ‘dangerous’ particles to present to the immune system. In CD, the HLA-DQ2/8 makes our MHC molecules extremely efficient in binding and presenting gluten as a ‘danger’ to the immune system. And the reason for this? We’re not sure yet – so far, all we can say about that is we have bad luck! So yes kids, technically, you can blame your parents for your gluten-hating immune system!
Viral triggers?
I’ve mentioned already how smart the immune system is at differentiating between what is ‘dangerous’ and ‘safe’ – and this is extremely important in the gut. We all know about the ‘friendly bacteria’ in our tummies, but we also have bad bacteria in there, and the immune system can tell them apart, under normal circumstances. However, if something were to disrupt the balance between the tolerance of the good microbes and the attacks against the bad, such as a viral infection, stress or hormonal changes, the previously dormant autoimmune responses towards gluten may become activated. However, for this to occur the individual must also have the specific HLA-DQ2/8 gene, as this is a requirement for coeliac disease to manifest itself.
Will there be a cure in the future?
Hopefully! However, at the moment, the only treatment available is a strict gluten-free diet. There are numerous studies being carried out by scientists around the world searching for the cure for coeliac disease. These include drugs that ‘mask’ gluten (thus no autoimmune response), prevent gluten from interacting with those APCs mentioned above, and even the growth of genetically modified grains with a less immunogenic form of gluten which coeliacs may be able to tolerate. This is all rather theory based at the moment, and a cure for CD is still a distant dream – but let’s stay optimistic. Until then, we’re stuck with our lives of crumbly bread and rice cakes.
 Michelle Kickham is a doctoral candidate in Immunology and Organic Chemistry and a current Irish Research Council scholar. Michelle believes that science holds the power to make a real difference and her goal is to explain the science behind health claims, offer advice and tips, as well as sharing healthy recipes to suit almost any diet.
Michelle Kickham is a doctoral candidate in Immunology and Organic Chemistry and a current Irish Research Council scholar. Michelle believes that science holds the power to make a real difference and her goal is to explain the science behind health claims, offer advice and tips, as well as sharing healthy recipes to suit almost any diet.
For more information, visit www.gfandallthingsnice.wordpress.com
